Diabetic retinopathy diagnosis and Management...
Contents
- Structure and function of the eye
- Definition and classification of diabetic retinopathy
- Risk factors for diabetic retinopathy
- Diagnosis of retinopathy
- Laser treatment for diabetic retinopathy
- Surgery for retinopathy
STRUCTURE AND FUNCTION OF THE EYE
The eye is similar to a camera. It has a clear lens
focussing light to a light sensitive membrane (the retina) which creates nerve
signals. These signals form the basis of vision and are sent to the brain via
the optic nerves. The brain processes the signals and eyesight is perceived by
the individual.
The retina is a thin transparent membrane spread
over the inside of the back of the eye. It contains specialised cells called
rods and cones and it is these cells that register the light. The cone cells
are responsible for clear, straight ahead viewing and colour vision. The rod
cells provide night and side vision. The retina is kept alive by blood vessels
both within its structure and underneath it. The blood vessels are known as
retinal arteries, capillaries and veins. Clearly anything that interferes with
the function of the retina will have some impact on eyesight.
The most important part of the retina is where the cone cells are and this is called the macula. It represents the centre of vision.
DEFINITION AND CLASSIFICATION OF DIABETIC
RETINOPATHY
In people with diabetes the capillaries in the
retina are diseased and damaged. These damaged vessels either leak or become
completely blocked. This is diabetic retinopathy and it has a number of effects
that can lead to vision loss. It is a slow process taking months to years to
have its effects.
Early diabetic retinopathy is called
non-proliferative diabetic retinopathy. More advanced disease is called
proliferative diabetic retinopathy. A common process seen in diabetes is called
diabetic macular oedema where the macula swells.
RISK FACTORS FOR DIABETIC RETINOPATHY
The longer a person has had diabetes the greater
the risk of diabetic retinopathy. About 80% of people who have diabetes for 15
years will have some retinopathy. However, about 13% of newly diagnosed adults
will have retinopathy at the time of diagnosis.
The consistency of good control of sugar during
diabetes also impacts on the development and severity of diabetic retinopathy.
High blood pressure, kidney failure and cholesterol
can adversely affect the severity of diabetic retinopathy.
Pregnancy can sometimes result in a rapid
acceleration of diabetic retinopathy.
For all these reasons, a newly diagnosed adult
should have a full eye examination at the time of diagnosis and then one to two
yearly thereafter. A child who develops diabetes need not be examined at
diagnosis but should have an eye examination after 5 years of disease. An
insulin dependent female planning pregnancy should have an eye examination at
three months into pregnancy.
Smoking does accelerate the damage diabetes does to
the retina. A person with diabetic retinopathy should not smoke. Nor should
anyone else.
DIAGNOSIS OF DIABETIC
RETINOPATHY
SYMPTOMS
Blurring of vision is the main symptom associated
with diabetic retinopathy but this usually occurs when the disease is already
well established. Many people with diabetic retinopathy will have no symptoms
at all. Diabetic retinopathy does not cause pain. People with proliferative
retinopathy may experience floating spots in their vision due to bleeding
within the eye.
The doctor will take your full medical history
including all other health problems, medications, allergies. Your vision will
be measured.
SIGNS
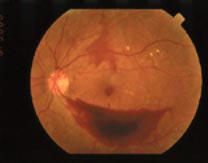
Your eye doctor will examine your eyes and should
use drops to dilate or open the pupils. The doctor will be able to examine the
retina in detail. A photo of a normal retina is seen below.
If the retina is diseased then the doctor may carry
out a test known as fluorescein angiography. This is a photographic record of
the state of the retinal blood vessels. A yellow dye is injected into an arm
vein and photographs using a special camera are taken.
A normal photograph from a fluorescein angiogram is
depicted below.
The eye examination and tests will enable the eye
doctor to determine the extend and severity of diabetic retinopathy. Treatment
recommendations can be made.
In early non-proliferative diabetic retinopathy,
most people usually have no symptoms and there are small areas of leakage in
the retina.
If diabetic macular oedema occurs, then laser
treatment may be needed.
More established non-proliferative retinopathy may
require careful monitoring or laser treatment.
In proliferative diabetic retinopathy, much of the retina is affected by obstruction of retinal capillaries. This may not necessarily affect vision directly but it does cause new capillaries to grow on the surface of the retina or optic nerve.
These new vessels are prone to bleeding and can fill the eye with blood, dramatically blurring vision. In addition, scar tissue can develop causing retinal detachment to occur.
TREATMENT OF DIABETIC RETINOPATHY
Improvement of diabetic control, reduction of risk
factors such as high blood pressure and cholesterol and regular eye
examinations will all help toward reducing the impact of diabetic retinopathy
on a person’s eyesight.
The two treatments for diabetic retinopathy, once
established, are:
- laser
- vitrectomy surgery
Neither of these treatments cures retinopathy. The
best that can be achieved usually is slowing or preventing further vision loss.
LASER TREATMENT FOR DIABETIC RETINOPATHY
Laser treatment is usually indicated to control
leakage from capillaries in diabetic macular oedema, or to shrink new vessels
in proliferative diabetic retinopathy. In diabetic macular oedema, small
applications of laser are used to cauterise the leaking vessels using thermal
energy. In proliferative retinopathy, more intensive treatments to much of the
retina are required to shrink the new vessels.
Laser treatment may be associated with discomfort
or pain. Some treatments may require pain relieving medication or anaesthetic
injections to numb the eye. Eyesight may fluctuate during a course of
treatment.
SURGERY FOR RETINOPATHY
Vitrectomy surgery is required for advanced cases
of proliferative diabetic retinopathy. When there has been severe bleeding into
the eye which has not resolved spontaneously, then the blood (contained with
the normal vitreous gel) is removed using fine instruments. The instruments are
passed through small cuts in the white part of the eye. If the retina is
detached then  scar tissue is cut and peeled away from the retina. The
vitreous gel does not regrow and your eye does not require the gel for vision.
Typically the gel is replaced at the time of surgery with fluid, gas or liquid
silicone. Laser and cryotherapy may be used during surgery. Cataract surgery may
be required at the time of vitrectomy surgery. Surgery can take one to four
hours depending on complexity. Following surgery there will be a gradual
improvement in vision over the coming weeks to months. You will need to use
eyedrops for 4-6 weeks after surgery.
COMPLICATIONS OF LASER TREATMENT
Discomfort and pain
Fluctuating vision
Some loss of side and night vision
Some loss of colour vision
Slight risk of inadvertent damage to the macula
which could reduce central vision
[diag&mgt13]
COMPLICATIONS OF SURGICAL TREATMENT
The retina itself may be damaged during the
procedure necessitating further surgery
Cataract
Further bleeding into the eye after surgery
Reduction in overall quality of vision
Infection
Complications associated with anaesthesia.
You should discuss the risk of complications with
your eye doctor.











Comments
Post a Comment
If you have any questions, Please let me know